What Are The Main Reasons For Over-Pronation Of The Foot
Overpronation is a term which is used more and more frequently by runners and exercisers these days, but what is overpronation and is it bad? Overpronation is excessive pronation of the feet when walking and running, and it can place people at risk of developing foot problems. Knowing the degree to which you pronate is important in order to select the correct footwear and exercise shoes. If you pronate excessively you could be placing an excessive strain on your feet, however overpronators can also place an excessive strain on the ankles, legs, knees, hips and lower back. Runners often claim to be an overpronator or even an underpronator or supinator. These terms may very well be viewed in a negative light when they really are not a problem at all. On the other hand people may be overpronators and not even know about it and could be at a high risk of developing a musculoskeletal problem.

Causes
Generally fallen arches are a condition inherited from one or both parents. In addition, age, obesity, and pregnancy cause our arches to collapse. Being in a job that requires long hours of standing and/or walking (e.g. teaching, retail, hospitality, building etc) contributes to this condition, especially when standing on hard surfaces like concrete floors. Last, but not least unsupportive footwear makes our feet roll in more than they should.
Symptoms
When standing, your heels lean inward. When standing, one or both of your knee caps turn inward. Conditions such as a flat feet or bunions may occur. You develop knee pain when you are active or involved in athletics. The knee pain slowly goes away when you rest. You abnormally wear out the soles and heels of your shoes very quickly.
Diagnosis
Bunions, calluses and crooked toes may indicate alignment problems. So, it is important to ascertain the condition of a client's toes. Check the big toe to determine if the first joint of the toe is swollen, has a callus or bunion, and/or looks as though it abducts (i.e., hallux valgus) rather than pointing straight ahead. Also, look to see if the lesser toes seem to "curl up" (i.e., the person has hammer or claw toes). This may be indicative of damage to, or inflexibility of the plantar fascia caused by excessive flattening of the foot.

Non Surgical Treatment
Adequate footwear can often help with conditions related to flat feet and high arches. Certified Pedorthists recommend selecting shoes featuring heel counters that make the heel of the shoe stronger to help resist or reduce excessive rearfoot motions. The heel counter is the hard piece in the back of the shoe that controls the foot?s motion from side-to-side. You can quickly test the effectiveness of a shoe?s heel counter by placing the shoe in the palm of your hand and putting your thumb in the mid-portion of the heel, trying to bend the back of the shoe. A heel counter that does not bend very much will provide superior motion control. Appropriate midsole density, the firmer the density, the more it will resist motion (important for a foot that overpronates or is pes planus), and the softer the density, the more it will shock absorb (important for a cavus foot with poor shock absorption) Wide base of support through the midfoot, to provide more support under a foot that is overpronated or the middle of the foot is collapsed inward.
Prevention
Many of the prevention methods for overpronation-orthotics, for example-can be used interchangeably with treatment methods. If the overpronation is severe, you should seek medical attention from a podiatrist who can cast you for custom-made orthotics. Custom-made orthotics are more expensive, but they last longer and provide support, stability, and balance for the entire foot. You can also talk with a shoe specialist about running shoes that offer extra medial support and firm heel counters. Proper shoes can improve symptoms quickly and prevent them from recurring. Surgery can sometimes help cure and prevent this problem if you suffer from inherited or acquired pes planus deformity. Surgery typically involves stabilizing the bones to improve the foot?s support and function.
Could I Take Care Of Calcaneal Apophysitis In The Home?
Although the name might sound pretty frightening, Sever's disease is really a common heel injury that occurs in kids. It can be painful, but is only temporary and has no long-term effects. Calcaneal apophysitis is a painful inflammation of the heel?s growth plate. It typically affects children between the ages of 8 and 14 years old, because the heel bone (calcaneus) is not fully developed until at least age 14. Until then, new bone is forming at the growth plate (physis), a weak area located at the back of the heel. When there is too much repetitive stress on the growth plate, inflammation can develop. Calcaneal apophysitis is also called Sever?s disease, although it is not a true ?disease.? It is the most common cause of heel pain in children, and can occur in one or both feet. Heel pain in children differs from the most common type of heel pain experienced by adults. While heel pain in adults usually subsides after a period of walking, pediatric heel pain generally doesn?t improve in this manner. In fact, walking typically makes the pain worse.
Causes
Apart from the age of the young person, other factors that may contribute to developing the disease may include; overuse or too much physical activity. Your child?s heel pain may be caused by repeated stress on the heels (running and jumping activities), pressure on the back of the heel from too much standing or wearing poor-fitting shoes. This includes shoes that do not support or provide enough padding for your child?s feet.
Symptoms
Symptoms of calcaneal apophysitis may include pain in the back or bottom of the heel, Limping, walking on toes, difficulty running, jumping, or participating in usual activities or sports. Pain when the sides of the heel are squeezed.
Diagnosis
Sever?s disease can be diagnosed based on your history and symptoms. Clinically, your physiotherapist will perform a "squeeze test" and some other tests to confirm the diagnosis. Some children suffer Sever?s disease even though they do less exercise than other. This indicates that it is not just training volume that is at play. Foot and leg biomechanics are a predisposing factor. The main factors thought to predispose a child to Sever?s disease include decrease ankle dorsiflexion, abnormal hind foot motion eg overpronation or supination, tight calf muscles, excessive weight-bearing activities eg running.
Non Surgical Treatment
Activity Modification: to decrease the pain, limiting sporting activities is essential. Cutting back on the duration, intensity, and frequency can significantly improve symptoms. Heel cord stretching is important if heel cord tightness is present. Heel cushions/cups or soft orthotics decreases the impact on the calcaneus by distributing and cushioning the weight bearing of the heel. Use of NSAIDS. Ibuprofen (Nuprin, Motrin) or naproxen (Aleve) can decrease pain and secondary swelling. Ice. Placing cold or ice packs onto the painful heel can alleviate pain. Short-leg cast. For recalcitrant symptoms a short-leg cast is occasionally used to force rest the heel.
Prevention
Treat symptoms when they occur with RICE and NO HARM. RICE (Rest Ice, Compression and Elevation) will help following activity and when symptoms flare, while No HARM (No Heat, alcohol, running or massage) will help reduce the symptoms from occurring. Orthotics. The use of an Interpod Orthotic will assist in realigning the foot, which will reduce the stress on the Achilles Tendon and prevent reoccurring symptoms. The orthotic achieves this by reducing the forces and stress placed on the limbs during walking and running. Exercise reduction. Patients may need to reduce their level of activity if this is seen as a contributing factor. Training errors. Ensue athletes warm up and cool down correctly with stretching activities. Footwear. Sporting and school shoes should have an appropriate heel height to assist in offloading of the Achilles tendon.
Acquired Flat Foot Deformity
Overview
Most flat feet are not painful, particularly those flat feet seen in children. In the adult acquired flatfoot, pain occurs because soft tissues (tendons and ligaments) have been torn. The deformity progresses or worsens because once the vital ligaments and posterior tibial tendon are lost, nothing can take their place to hold up the arch of the foot. The painful, progressive adult acquired flatfoot affects women four times as frequently as men. It occurs in middle to older age people with a mean age of 60 years. Most people who develop the condition already have flat feet. A change occurs in one foot where the arch begins to flatten more than before, with pain and swelling developing on the inside of the ankle. Why this event occurs in some people (female more than male) and only in one foot remains poorly understood. Contributing factors increasing the risk of adult acquired flatfoot are diabetes, hypertension, and obesity. 
Causes
The cause of posterior tibial tendon insufficiency is not completely understood. The condition commonly does not start from one acute trauma but is a process of gradual degeneration of the soft tissues supporting the medial (inner) side of the foot. It is most often associated with a foot that started out somewhat flat or pronated (rolled inward). This type of foot places more stress on the medial soft tissue structures, which include the posterior tibial tendon and ligaments on the inner side of the foot. Children nearly fully grown can end up with flat feet, the majority of which are no problem. However, if the deformity is severe enough it can cause significant functional limitations at that age and later on if soft tissue failure occurs. Also, young adults with normally aligned feet can acutely injure their posterior tibial tendon from a trauma and not develop deformity. The degenerative condition in patients beyond their twenties is different from the acute injuries in young patients or adolescent deformities, where progression of deformity is likely to occur.
Symptoms
The first stage represents inflammation and symptoms originating from an irritated posterior tibial tendon, which is still functional. Stage two is characterized by a change in the alignment of the foot noted on observation while standing (see above photos). The deformity is supple meaning the foot is freely movable and a ?normal? position can be restored by the examiner. Stage two is also associated with the inability to perform a single-leg heel rise. The third stage is dysfunction of the posterior tibial tendon is a flatfoot deformity that becomes stiff because of arthritis. Prolonged deformity causes irritation to the involved joints resulting in arthritis. The fourth phase is a flatfoot deformity either supple (stage two) or stiff (stage 3) with involvement of the ankle joint. This occurs when the deltoid ligament, the major supporting structure on the inside of the ankle, fails to provide support. The ankle becomes unstable and will demonstrate a tilted appearance on X-ray. Failure of the deltoid ligament results from an inward displacement of the weight bearing forces. When prolonged, this change can lead to ankle arthritis. The vast majority of patients with acquired adult flatfoot deformity are stage 2 by the time they seek treatment from a physician.
Diagnosis
In diagnosing flatfoot, the foot & Ankle surgeon examines the foot and observes how it looks when you stand and sit. Weight bearing x-rays are used to determine the severity of the disorder. Advanced imaging, such as magnetic resonance imaging (MRI) and computed tomography (CAT or CT) scans may be used to assess different ligaments, tendons and joint/cartilage damage. The foot & Ankle Institute has three extremity MRI?s on site at our Des Plaines, Highland Park, and Lincoln Park locations. These extremity MRI?s only take about 30 minutes for the study and only requires the patient put their foot into a painless machine avoiding the uncomfortable Claustrophobia that some MRI devices create.
Non surgical Treatment
Depending on the stage of the deformity and patient?s functional goals, various treatment options are available. Some patients improve with conservative care which includes rest and immobilization, shoe modifications, orthoses and bracing, or physical therapy. Surgery might be warranted for advanced stages of the condition. Often a combination of procedures including tendon and muscle augmentation, tendon transfers, realigning of bones or fusion of certain joints might be necessary in more advanced cases. Your doctor will evaluate and recommend an individualized plan of care with your specific needs in mind. 
Surgical Treatment
If initial conservative therapy of posterior tibial tendon insufficiency fails, surgical treatment is considered. Operative treatment of stage 1 disease involves release of the tendon sheath, tenosynovectomy, debridement of the tendon with excision of flap tears, and repair of longitudinal tears. A short-leg walking cast is worn for 3 weeks postoperatively. Teasdall and Johnson reported complete relief of pain in 74% of 14 patients undergoing this treatment regimen for stage 1 disease. Surgical debridement of tenosynovitis in early stages is believed to possibly prevent progression of disease to later stages of dysfunction.
What Can Cause Arch Pain ?
Arch pain typically is the term used to describe pain under the arch of the foot. Arch pain indicates inflammation of the tissues within the midfoot and is most commonly caused by plantar fasciitis. Plantar fasciitis is inflammation of the fibrous band of tissue that connects the heel to the toes. Arch pain is most commonly found early in the morning due to the plantar fascia becoming contracted and tight during sleep. Walking or standing for long periods of time can also aggravate the plantar fascia, causing it to become inflamed and irritated. Treatment options include orthotics, anti-inflammatory medications and stretching exercises.

Causes
The causes of high arched feet can vary greatly. They range from neurological disorders, club foot, injury, and often times there may be no known reason. The idea behind surgery to correct this often painful condition is to bring the arch down and thereby, allow the ground pressure of walking to be more evenly distributed across the entire bottom of the foot. Over time high arch feet can cause severe plantar calluses, ulcerations broken metatarsals and even chronically sprained ankles.
Symptoms
Flat feet don't usually cause problems, but they can put a strain on your muscles and ligaments (ligaments link two bones together at a joint). This may cause pain in your legs when you walk. If you have flat feet, you may experience pain in any of the following areas, the inside of your ankle, the arch of your foot, the outer side of your foot, the calf, the knee, hip or back, Some people with flat feet find that their weight is distributed unevenly, particularly if their foot rolls inwards too much (overpronates). If your foot overpronates, your shoes are likely to wear out quickly. Overpronation can also damage your ankle joint and Achilles tendon (the large tendon at the back of your ankle). See your GP if you or your child has flat feet and your feet are painful, even when wearing supportive, well-fitting shoes, shoes wear out very quickly, feet appear to be getting flatter, feet are weak, numb or stiff, Your GP may refer you to a podiatrist (foot specialist).
Diagnosis
The adult acquired flatfoot, secondary to posterior tibial tendon dysfunction, is diagnosed in a number of ways with no single test proven to be totally reliable. The most accurate diagnosis is made by a skilled clinician utilizing observation and hands on evaluation of the foot and ankle. Observation of the foot in a walking examination is most reliable. The affected foot appears more pronated and deformed compared to the unaffected foot. Muscle testing will show a strength deficit. An easy test to perform in the office is the single foot raise.
Non Surgical Treatment
There are many treatments for fasciitis. The most common initial treatment provided by the family doctor are anti-inflammatory medications. They may take the edge off the pain, but they don't often resolve the condition fully. Steroid injections, which deliver the medication directly to the most painful area, are usually more effective. Rest, ice, weight loss, taping, strapping, immobilization, physiotherapy, massage, stretching, heel cushions, acupuncture, night splints and extra-corporeal shock wave therapy all help some patients.

Surgical Treatment
If you have pain that has not been responsive to other treatments, there is a new non-surgical treatment that was recently approved by the FDA. ESWT (extracorporeal shockwave therapy) uses strong electrohydraulic acoustic (sound) energy that triggers the body?s natural repair mechanism. This treatment method is safe, effective and requires a very short recovery period compared to older surgical techniques.
Prevention
There are several things that you can do to prevent and treat arch pain. This includes Avoiding high heeled shoes, Stretching the calf muscles regularly, Wearing well fitted, comfortable shoes, Using customisedorthotic devices or shoe inserts, Elevating the feet and applying ice and taking over-the-counter anti-inflammatory medications. You can also care for your feet by paying attention to any changes in your feet as you get older. It is normal for feet to lose some of their fat pads as a person ages. Your feet may get bigger, both wider and longer as well. Make sure that you wear shoes that are sturdy, but comfortable, and have your feet measured before you buy shoes to make sure that you are still wearing the right size. Shoe sizes vary from one brand to the next, so it is a good idea to have your feet measured every time you purchase shoes. When choosing shoes, match the shoe to the activity for which it will be worn. Within the broader grouping of athletic shoes, there are different categories with different features. For example, a running shoe has different features than a walking shoe. You may develop some arthritic changes in your feet over time, too. If you notice that you are experiencing more pain in your feet, see your doctor for an evaluation. If the pain is arthritis-related, your doctor may recommend medication or other treatment to slow the progression of the arthritis.
Stretching Exercises
Achilles stretch. Stand with the ball of one foot on a stair. Reach for the step below with your heel until you feel a stretch in the arch of your foot. Hold this position for 15 to 30 seconds and then relax. Repeat 3 times. Balance and reach exercises. Stand next to a chair with your injured leg farther from the chair. The chair will provide support if you need it. Stand on the foot of your injured leg and bend your knee slightly. Try to raise the arch of this foot while keeping your big toe on the floor. Keep your foot in this position. With the hand that is farther away from the chair, reach forward in front of you by bending at the waist. Avoid bending your knee any more as you do this. Repeat this 15 times. To make the exercise more challenging, reach farther in front of you. Do 2 sets of 15. While keeping your arch raised, reach the hand that is farther away from the chair across your body toward the chair. The farther you reach, the more challenging the exercise. Do 2 sets of 15. Towel pickup. With your heel on the ground, pick up a towel with your toes. Release. Repeat 10 to 20 times. When this gets easy, add more resistance by placing a book or small weight on the towel. Resisted ankle plantar flexion. Sit with your injured leg stretched out in front of you. Loop the tubing around the ball of your foot. Hold the ends of the tubing with both hands. Gently press the ball of your foot down and point your toes, stretching the tubing. Return to the starting position. Do 2 sets of 15. Resisted ankle dorsiflexion. Tie a knot in one end of the elastic tubing and shut the knot in a door. Tie a loop in the other end of the tubing and put the foot on your injured side through the loop so that the tubing goes around the top of the foot. Sit facing the door with your injured leg straight out in front of you. Move away from the door until there is tension in the tubing. Keeping your leg straight, pull the top of your foot toward your body, stretching the tubing. Slowly return to the starting position. Do 2 sets of 15. Heel raise. Stand behind a chair or counter with both feet flat on the floor. Using the chair or counter as a support, rise up onto your toes and hold for 5 seconds. Then slowly lower yourself down without holding onto the support. (It's OK to keep holding onto the support if you need to.) When this exercise becomes less painful, try doing this exercise while you are standing on the injured leg only. Repeat 15 times. Do 2 sets of 15. Rest 30 seconds between sets.
Acquired Flat Foot Tibialis Posterior Exercises
Overview
Collapsed arches occur in five percent of adults 40 years and older, especially those who are overweight or maintain sedentary lifestyles. At the onset of the condition, adult acquired flatfoot can be controlled with anti-inflammatory medications, physical therapy, taping, bracing, and orthotics. While most cases of adult-onset flatfoot require surgery, congenital flatfoot is an entirely different condition that is best treated with orthotics in children. Ninety percent of children born with flat feet will be fine with conservative treatment. 
Causes
Posterior tibial tendon dysfunction is the most common cause of acquired adult flatfoot. Sometimes this can be a result of specific trauma, but usually the tendon becomes injured from wear and tear over time. This is more prevalent in individuals with an inherited flat foot but excessive weight, age, and level of activity are also contributing factors.
Symptoms
At first you may notice pain and swelling along the medial (big toe) side of the foot. This is where the posterior tibialis tendon travels from the back of the leg under the medial ankle bone to the foot. As the condition gets worse, tendon failure occurs and the pain gets worse. Some patients experience pain along the lateral (outside) edge of the foot, too. You may find that your feet hurt at the end of the day or after long periods of standing. Some people with this condition have trouble rising up on their toes. They may be unable to participate fully in sports or other recreational activities.
Diagnosis
The diagnosis of posterior tibial tendon dysfunction and AAFD is usually made from a combination of symptoms, physical exam and x-ray imaging. The location of pain, shape of the foot, flexibility of the hindfoot joints and gait all may help your physician make the diagnosis and also assess how advanced the problem is.
Non surgical Treatment
Patients can be treated non-surgically with in-shoe devices and braces to hold their feet in the correct position. This can reduce pain and damage and assist with walking. Physical therapy is also given to improve muscle strength and help prevent injury to the foot. Surgery can be performed if the patient doesn?t find any relief. 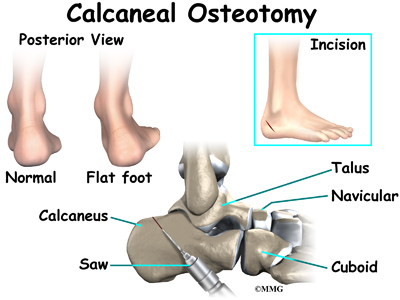
Surgical Treatment
Surgery is usually performed when non-surgical measures have failed. The goal of surgery is to eliminate pain, stop progression of the deformity and improve a patient?s mobility. More than one technique may be used, and surgery tends to include one or more of the following. The tendon is reconstructed or replaced using another tendon in the foot or ankle The name of the technique depends on the tendon used. Flexor digitorum longus (FDL) transfer. Flexor hallucis longus (FHL) transfer. Tibialis anterior transfer (Cobb procedure). Calcaneal osteotomy - the heel bone may be shifted to bring your heel back under your leg and the position fixed with a screw. Lengthening of the Achilles tendon if it is particularly tight. Repair one of the ligaments under your foot. If you smoke, your surgeon may refuse to operate unless you can refrain from smoking before and during the healing phase of your procedure. Research has proven that smoking delays bone healing significantly.